Once you're pregnant, early and regular prenatal care is important to keep yourself and your developing infant healthy.
During your first prenatal visit, your health care provider may talk to you about the following ways to help have a healthy pregnancy:1
Begin or continue to get at least 400 micrograms of folic acid by taking vitamin supplements every day to reduce your child's risk of neural tube defects. In the United States, enriched grain products such as bread, cereal, pasta, and other grain-based foods are fortified with folic acid. A related form, called folate, occurs naturally in leafy, green vegetables and orange juice, but folate is not absorbed as well as folic acid.2 Also, it can be difficult to get all the folic acid you need from food alone.3 Most prenatal vitamins contain 400 micrograms of folic acid.4 If you have had a child with an NTD before, taking a larger daily dose of folic acid (4 mg) before and during early pregnancy can reduce the risk for recurrence in a subsequent pregnancy.
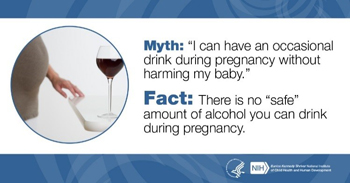 Drinking alcohol, smoking, and taking drugs during pregnancy can increase your child's risk for problems such as fetal alcohol spectrum disorders (FASDs), sudden infant death syndrome (SIDS), and other problems.5,6
Drinking alcohol, smoking, and taking drugs during pregnancy can increase your child's risk for problems such as fetal alcohol spectrum disorders (FASDs), sudden infant death syndrome (SIDS), and other problems.5,6
FASDs are a variety of effects on the fetus that result from the mother drinking alcohol during pregnancy. The effects range from mild to severe, and they include intellectual and developmental disabilities; behavior problems; abnormal facial features; and disorders of the heart, kidneys, bones, and hearing. FASDs last a lifetime although early intervention services can help improve a child's development. FASDs are completely preventable: If a woman does not drink alcohol while she is pregnant, her child will not have an FASD.7 Currently, research shows that there is no safe amount of alcohol to drink while pregnant. According to one recent study supported by the NIH, infants can suffer long-term developmental problems even with low levels of prenatal alcohol exposure.8
Other research shows that smoking tobacco, smoking marijuana, exposure to second-hand smoke, and taking drugs during pregnancy can also harm the fetus and affect infant health. One study showed that smoking tobacco or marijuana and using illegal drugs doubled or even tripled the risk of stillbirth, fetal death after 20 weeks of pregnancy.9 Likewise, drinking alcohol, smoking tobacco, and exposure to second-hand smoke during pregnancy increases the risk of SIDS, the sudden, unexplained death of an infant younger than 1 year old.10 Research also shows that smoking marijuana during pregnancy can interfere with normal brain development in the fetus, possibly causing long-term problems.11 For more information, visit https://www.drugabuse.gov/publications/research-reports/substance-use-in-women/
substance-use-while-pregnant-breastfeeding.
Your health care provider can be a source of help if you find it hard to quit smoking or drinking on your own. You can also visit http://smokefree.gov/ for plans and information about quitting smoking. The Rethinking Drinking website provides resources and information related to quitting alcohol use. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a services locator through its website at https://findtreatment.samhsa.gov/. SAMHSA also has a confidential hotline through which people can find assistance: 1-800-662-HELP (4357).
According to the CDC, most women take at least one medication during pregnancy.12 The majority of medications have not been specifically studied for use in pregnancy. Talk to your health care provider about over-the-counter and prescription medications and herbal and vitamin supplements. Certain medications to treat acne and epilepsy and some dietary or herbal supplements can harm the fetus during pregnancy.
Taking prescription pain medications, specifically opioids, during pregnancy can pose serious risks to the fetus. Taking these medications during pregnancy doubles or even triples the risk for stillbirth.9 If taken regularly during pregnancy, the baby may go through withdrawal after birth, a situation called neonatal abstinence syndrome (NAS). Babies with NAS face a variety of symptoms and problems, some of them severe.13 The best way to protect your baby from these problems is to stop taking these medications during pregnancy.
During pregnancy, exposure to radiation, pesticides, some metals, and certain chemicals can cause birth defects, premature birth, and miscarriage.14 If you're not sure if something might be harmful to you or your fetus, avoid contact with it until you check with your health care provider.
If you work in a job on a farm, a dry cleaner, a factory, a nail or hair salon, you might be around or come into contact with potentially harmful substances. Talk to your health care provider and your employer about how you can protect yourself before and during pregnancy. You may need extra protection at work or a change in your job duties to stay safe.14
A few examples of exposures that are known to be toxic to the developing fetus are:
Lead: Lead is a metal that may be present in house paint, dust, and garden soil. Any home built before 1978 may have lead paint. Exposure can occur when removing paint in old buildings (or if the paint is peeling) and working in some jobs (for example, manufacturing automotive batteries). Lead is also present in some well water and in water that travels through lead pipes. High levels of lead during pregnancy can cause miscarriage, stillbirth, low birth weight, and premature delivery, as well as learning and behavior problems for the child.15 Women who had exposure to lead in the past should have1 their blood levels checked before and during pregnancy.15 Call the National Lead Information Center for information about how to prevent exposure to lead at: 800-424-LEAD.
Radiation: Radiation is energy that travels through space. It can be in the form of X-rays, radio waves, heat, or light, or it can come from "radioactive" materials like dust, metals, or liquids that give off energy called radioactivity. Low exposures to radiation from natural sources (such as from the sun) or from microwave ovens or routine medical X-rays are generally not harmful. Because the fetus is inside the mother, it is partially protected from radiation's effects.14,16 Pregnant women or women who might be pregnant should make sure their dentists and doctors are aware of this so appropriate precautions can be taken with medical scans (X-rays or CT scans) or treatments that involve radiation.14 Pregnant women who may be exposed to radiation in the workplace should speak with their employer and health care provider to make sure the environment is safe during their pregnancy. Nuclear or radiation accidents, while rare, can cause high radiation exposures that are extremely dangerous, especially to the developing fetus.
Solvents: Solvents are chemicals that dissolve other substances. Solvents include alcohols, degreasers, and paint thinners. Some solvents give off fumes or can be absorbed through the skin and can cause severe health problems. During pregnancy, being in contact with solvents, especially if you work with them, can be harmful. Solvents may lead to miscarriage, slow the growth of the fetus, or cause preterm birth and birth defects.14 Pregnant women who may be exposed to solvents in the workplace should speak with their employer and health care provider to make sure the environment is safe during their pregnancy.17 Whenever you use solvents, be sure to do so in a well-ventilated area, wear safety clothes (such as gloves and a face mask), and avoid eating and drinking in the work area.14
Many chemicals are commonly found in the blood and body fluids of pregnant women and their infants. However, much remains unknown about the effects of fetal exposure to chemicals.18 It's best to be cautious about chemical exposure when you are planning to get pregnant or if you are pregnant. Talk to your health care provider if you live or work in or near a toxic environment.17
Choose a variety of fruits, vegetables, whole grains, and low-fat dairy products to help ensure the developing fetus gets all the nutrients it needs. Make sure you also drink plenty of water. An online tool called the Daily Checklist for Moms can help you plan your meals so that you get the right foods in the right amounts according to your personal characteristics and your stage of pregnancy.
Read Nutrition During Pregnancy FAQs ![]() (PDF – 72.1 KB) from the American College of Obstetricians and Gynecologists to learn more about how much you should eat during pregnancy, the nutrients you need, and how much caffeine is safe to drink.
(PDF – 72.1 KB) from the American College of Obstetricians and Gynecologists to learn more about how much you should eat during pregnancy, the nutrients you need, and how much caffeine is safe to drink.
Avoid certain foods such as raw fish, undercooked meat, deli meat, and unpasteurized cheeses (for example, certain types of feta, bleu cheese, and Mexican-style soft cheeses).19 Always check the label to make sure the cheese is pasteurized.
Some pregnant women are concerned about the amount of fish they can safely consume. Certain fish contain methylmercury, when certain bacteria cause a chemical change in metallic mercury. Methylmercury is found in foods that fish eat, and it remains in the fish's body after it is eaten. Methylmercury in fish eaten by pregnant women can harm a fetus's developing nervous system.
According to the U.S. Food and Drug Administration (FDA), pregnant women can eat up to 12 ounces a week of fish and shellfish that have low levels of methylmercury (salmon, canned light tuna, and shrimp). Albacore ("white") tuna has more methylmercury than canned light tuna; pregnant women should consume 6 ounces or less in a week. Avoid fish with high levels of methylmercury (swordfish, king mackerel, and shark). For more information on methylmercury and pregnancy, see the FDA Food Safety for Moms-to-Be.19
Some studies suggest that too much caffeine can increase the risk of miscarriage. Talk to your health care provider about the amount of caffeine you get from coffee, tea, or soda. Your health care provider might suggest a limit of 200 milligrams (the amount in about one 12-ounce cup of coffee) per day. Keep in mind, though, that some of the foods you eat, including chocolate, also contain caffeine and contribute to the total amount you consume each day.20
Most women can continue regular levels of physical activity throughout pregnancy. Regular physical activity can help you feel better, sleep better, and prepare your body for birth. After your child is born, it can help get you back to your pre-pregnancy shape more quickly.21 Talk to your health care provider about the amount and type of physical activity that is right for you.
Gaining too much or too little weight during pregnancy increases the risk of problems for both the mother and the infant. Following a healthy diet and getting regular physical activity can help you stay within the recommended weight gain guidelines set by the Institute of Medicine.
The amount of weight you should gain during pregnancy depends on your pre-pregnancy weight and body mass index (BMI), which is your weight in kilograms divided by the square of your height in meters (kg/m2). The following guidelines are for women who are pregnant with one fetus. The recommendations are different if you are pregnant with more than one fetus (such as twins).22,23
- Women who are underweight (BMI less than 18.5) should gain between 28 and 40 pounds.
- Women at a normal weight (BMI between 18.5 and 24.9) should gain between 25 and 35 pounds.
- Women with overweight (BMI 25 to 29.9) should gain between 15 and 25 pounds.
- Women with obesity (BMI more than 30) should gain between 11 and 20 pounds.
In a recent NICHD study of more than 8,000 pregnant women, 73% gained more than the recommended amount of weight. The study found that excessive weight gain during pregnancy increases the risk for gestational high blood pressure, cesarean section, and large-for-gestational-age infants.24
Talk to your health care provider about the right amount of weight gain for you based on your pre-pregnancy weight.
Iron-deficiency anemia—when the body doesn't have enough iron—is common during pregnancy and is associated with preterm birth and low birth weight. Your health care provider may screen you for iron-deficiency anemia and, if you have it, may recommend iron supplements.25 Your health care provider may also recommend a vitamin B12 supplement if you are a vegan.26,27 (Vegetarians normally get enough vitamin B12 by eating eggs and dairy products.)
Your gums are more likely to become inflamed or infected because of hormonal changes and increased blood flow during pregnancy.28 Make sure you tell your dentist if you think you could be pregnant, but keeping up your regularly scheduled checkups is important. Some women may fear getting dental work during pregnancy, but a 2006 study and 2011 follow-up study showed no increase in preterm births or other adverse outcomes for pregnant women who received dental care.29
Certain infections can affect pregnancy or the developing fetus. It's important to take steps to prevent such infections or get medical treatment before or during pregnancy.
Vaccinations can protect against many infections that can affect the mother's health, the pregnancy, the fetus, and even her newborn child. Some vaccines need to be given before pregnancy, so it's a good idea to review your vaccination history with your health care provider as part of your pre-pregnancy care. The Centers for Disease Control and Prevention provides recommendations about timing of vaccinations to help ensure a healthy pregnancy.
Learn more about how infections can affect pregnancy and which infections can cause problems during pregnancy.
Citations
- March of Dimes. (2011). Your first prenatal care checkup. Retrieved January 5, 2016, from http://www.marchofdimes.org/pregnancy/your-first-prenatal-care-checkup.aspx
- NIH Office of Dietary Supplements. (2016). Dietary supplement fact sheet: Folate. Retrieved January 5, 2016, from http://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- KidsHealth from Nemours. (Reviewed October 2014). Folic acid and pregnancy. Retrieved January 5, 2016, from http://kidshealth.org/parent/pregnancy_center/your_pregnancy/preg_folic_acid.html
- Womenshealth.gov. (2012). ePublications: Prenatal care fact sheet. Retrieved June 27,2017, from https://www.womenshealth.gov/a-z-topics/prenatal-care
- Centers for Disease Control and Prevention. (2015). Preconception health and health care: Planning for pregnancy. Retrieved January 5, 2016, from http://www.cdc.gov/preconception/planning.html
- American College of Obstetricians and Gynecologists. (2015). Marijuana use during pregnancy and lactation. Committee Opinion No. 637. Obstetrics and Gynecology, 126, 234–238. Retrieved November 9, 2016, from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/10/marijuana-use-during-pregnancy-and-lactation
- Centers for Disease Control and Prevention. (2015). Fetal alcohol spectrum disorders (FASDs): Facts about FASDs. Retrieved January 5, 2016, from http://www.cdc.gov/ncbddd/fasd/facts.html
- Eckstrand, K. L., Ding, Z., Dodge, N. C., Cowan, R. L., Jacobson, J. L., Jacobson, S.W., et al. (2012). Persistent dose-dependent changes in brain structure in young adults with low-to-moderate alcohol exposure in utero. Alcoholism: Clinical and Experimental Research, 36(11), 1892–1902. PMID: 22594302
- NICHD.(2013). Tobacco, drug use in pregnancy can double risk of stillbirth. Retrieved November 9, 2016, from https://www.nichd.nih.gov/news/releases/Pages/
121113-stillbirth-drug-use.aspx - NICHD.(2016). Ways to reduce the risk of SIDS and other sleep-related causes of infant death. Retrieved June 2, 2016, from https://www.nichd.nih.gov/sts/about/risk/Pages/reduce.aspx
- NICHD.(2016). Prenatal exposure to marijuana may disrupt fetal brain development, mouse study suggests. Retrieved November 9, 2016, from https://www.nichd.nih.gov/news/releases/Pages/
031516-prenatal-exposure-marijuana.aspx - Centers for Disease Control and Prevention. (2018). Treating for Two: Medicine and Pregnancy. Retrieved May 16, 2018, from https://www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- Patrick, S. W., Dudley, J., Martin, P. R., Harrell, F. E., Warren, M. D., Hartmann, K. E., et al. (2015). Prescription opioid epidemic and infant outcomes. Pediatrics, 135(5), 842–850. Retrieved November 9, 2016, from https://pediatrics.aappublications.org/content/early/2015/04/08/peds.2014-3299
- March of Dimes (2016). Is it safe? Retrieved January 5, 2016, from http://www.marchofdimes.com/pregnancy/stayingsafe_indepth.html
- Organization of Teratology Information Specialists. (2014). Lead and pregnancy. Retrieved January 5, 2016, from http://mothertobaby.org/fact-sheets/lead-pregnancy/pdf
(PDF 247 KB)
- Centers for Disease Control and Prevention. (2014). Cancer and long-term health effects of radiation exposure and contamination. Retrieved January 5, 2016, from https://www.cdc.gov/radiation-emergencies/signs-symptoms/cancer-long-term-health-effects.html
- University of California, San Francisco. (2010). Toxic matters: Protecting our families from toxic substances. Retrieved May 18, 2012, from https://prhe.ucsf.edu/
- Lanphear, B. P., Vorhees, C. V., & Bellinger, D. C. (2005). Protecting children from environmental toxins. PLOS Medicine, 2(3), e61.
- U.S. Food and Drug Administration. (2014). Food safety for moms-to-be: While you're pregnant—methylmercury. Retrieved January 6, 2016, from https://www.fda.gov/food/people-risk-foodborne-illness/food-safety-moms-be
- American College of Obstetricians and Gynecologists (ACOG).(2010). Moderate caffeine consumption during pregnancy [ACOG Committee Opinion]. Retrieved May 21, 2012, from http://www.acog.org/Resources_And_Publications/Committee_Opinions/
Committee_on_Obstetric_Practice/Moderate_Caffeine_Consumption_During_Pregnancy - KidsHealth from Nemours. (2014). Exercising during pregnancy. Retrieved January 5, 2016, from http://kidshealth.org/parent/pregnancy_center/your_pregnancy/exercising_pregnancy.html
- Institute of Medicine and National Research Council. (2009). Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: National Academies Press. Retrieved June 22, 2016, from http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/
2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines/
Report%20Brief%20-%20Weight%20Gain%20During%20Pregnancy.pdf(PDF 717 KB)
- American College of Obstetricians and Gynecologists (ACOG). (2013). Weight gain during pregnancy [ACOG Committee Opinion]. Retrieved May 30, 2013, from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/01/weight-gain-during-pregnancy
- Johnson, J., Clifton, R. G., Roberts, J. M., Myatt. L., Hauth, J. C., Spong, C. Y., et al. (2013). Pregnancy outcomes with weight gain above or below the 2009 Institute of Medicine guidelines. Obstetrics and Gynecology, 121(5), 969–975. PMID: 23635732
- Allen, L. H. (2000). Anemia and iron deficiency: effects on pregnancy outcome. American Journal of Clinical Nutrition, 71(5), 1280s–1284s. Retrieved November 9, 2016, from https://academic.oup.com/ajcn/article/71/5/1280S/4729385
- U.S.Department of Agriculture & U.S. Department of Health and Human Services. (2010). Dietary guidelines for Americans 2010. Retrieved May 21, 2012, from https://health.gov/sites/default/files/2020-01/DietaryGuidelines2010.pdf (PDF 2.89 MB)
- NICHD. (2010). Pregnancy and healthy weight. Retrieved April 10, 2012, from http://www.nichd.nih.gov/news/resources/spotlight/Pages/040710-pregnancy-healthy-weight.aspx
- March of Dimes. (2016). Gum and teeth change. Retrieved January 5, 2016, from http://www.marchofdimes.com/pregnancy/yourbody_teeth.html
- National Child and Maternal Oral Health Resource Center. (n.d.) Oral Health Care During Pregnancy: A Consensus Statement. Retrieved June 24, 2020, from https://www.mchoralhealth.org/materials/consensus_statement.php.

 BACK TO TOP
BACK TO TOP