NICHD’s portfolio on Cushing syndrome covers a range of topics, including diagnostic tests, at-risk populations, management of the syndrome in pregnancy, and health issues after successful treatment. NICHD is also involved with research training and the development of a scientific infrastructure to help broaden the reach of research in Cushing syndrome and other pituitary and adrenal gland disorders.
Through its many organizational units and research projects, NICHD research on Cushing syndrome includes some of the following:
- Screening and diagnosis. Cushing syndrome has symptoms in common with many other conditions and can be difficult to detect. Targeted screening of individuals with conditions that pose particular diagnostic difficulties—such as obesity or pregnancy—and improving diagnostic tools will enhance detection of the syndrome and facilitate earlier treatment. For example, NICHD is investigating whether it is effective to introduce widespread screening for Cushing syndrome in people with metabolic syndrome. Metabolic syndrome describes a group of factors, such as extra weight around the middle and insulin resistance, that can increase a person’s risk for diabetes and heart disease. Although screening tests in this population can identify some people with Cushing syndrome, the tests also misidentify many others. It is important to determine whether widespread screening is helpful overall.
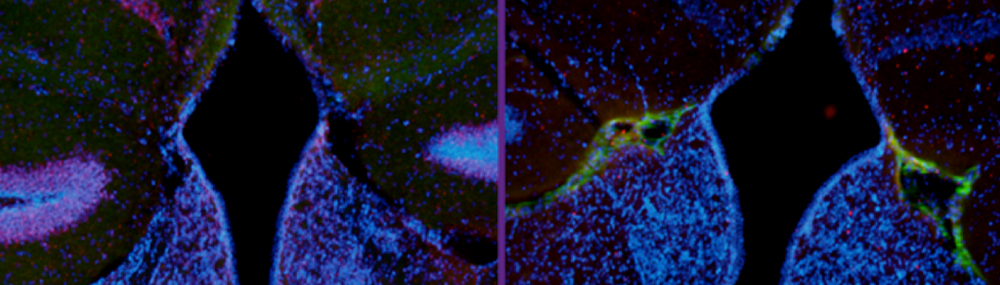
- Genetic disorders of the adrenal glands. Some genetic disorders, such as Carney complex and multiple endocrine neoplasia syndrome, raise an individual’s likelihood of developing Cushing syndrome. NICHD researchers are working to understand the genetic and molecular mechanisms of disorders that affect the adrenal cortex and pituitary gland and, ultimately, to prevent or cure them.
- Post-treatment health. Most people with Cushing syndrome can be cured and their cortisol levels will revert to normal. However, some individuals might take a while to recover to their previous levels of health, and they might never regain their full strength in some areas. NICHD researchers are investigating various aspects of post-treatment health. Their discoveries will help guide practice recommendations to ensure patients receive appropriate care, as needed, in the years after their initial Cushing syndrome treatment.
In Cushing syndrome, the earlier treatment begins, the less harmful the disease is to the body. However, Cushing syndrome is complex and difficult to diagnose. It has a wide range of symptoms that mimic those of other conditions, and the severity of the syndrome can fluctuate. Through its numerous research projects, NICHD aims to improve understanding of Cushing syndrome and, ultimately, to bring faster diagnoses and more effective treatment.
Institute Activities and Advances
NICHD’s Section on Endocrinology and Genetics (SEGEN), in the Division of Intramural Research, is working on ways to identify genes that might be involved—and how that involvement unfolds—in increasing the risk for Cushing syndrome. This can be seen with several disorders of the adrenal and pituitary glands as well as for multiple endocrine neoplasia syndromes that involve those glands. Researchers also are studying lingering and long-term effects from Cushing syndrome even after successful treatment. For example, Cushing syndrome might affect cognition permanently, so SEGEN researchers investigated memory impairment and depression in children. They found that some children are at risk for declines in intelligence measures and school performance even after successful treatment of their Cushing syndrome.
Additional NICHD research aims to develop new tests and tools to help healthcare providers screen for and diagnose individuals with Cushing syndrome. Previous NICHD research helped established the corticotropin-releasing hormone test and inferior petrosal sinus sampling as major diagnostic tools for identifying pituitary adenomas causing Cushing syndrome. Current research is evaluating the utility of hair samples for diagnosis.
Recent NICHD science advances related to Cushing syndrome include the following:
- Cushing syndrome patients have differences in blood clotting factors. Cushing syndrome patients with pituitary tumors are at higher risk for blood clots than those with adrenal tumors. To find out why, researchers investigated the levels of clotting factors in these two types of patients. (PMID: 28226363)
- Hair analysis may help diagnose Cushing syndrome. Researchers found that measuring cortisol levels in hair samples correlated with standard techniques for diagnosing Cushing syndrome. Although more work is needed, hair analysis may offer a reliable, less invasive diagnostic test in the future. (PMID: 28194652)
- Mutations in a particular gene can cause Cushing disease. The gene CABLES1 is involved in regulating the adrenal and pituitary glands. If this gene is mutated so it doesn’t function anymore, Cushing disease can result. (PMID: 28533356)
- Certain DNA changes are associated with food-dependent Cushing syndrome. Some people with Cushing syndrome make too much cortisol because of a problem with certain proteins that respond to food. Researchers studied how this works, using samples from 15 patients. (PMID: 28931750)
Other Activities and Advances
To achieve its goals for Cushing syndrome research, NICHD supports several research and clinical training programs for physicians. These programs are part of NIH-wide or other collaborative efforts in which NICHD participates. The following are examples.
- The Pediatric Endocrinology Training Program fellowship is a 3-year program accredited by the Accreditation Council for Graduate Medical Education. It provides comprehensive training in clinical patient management and guidance in the development of research skills. The fellowship is at NICHD and based at the NIH Clinical Center, which maintains clinical research protocols investigating the treatment of adrenal and pituitary tumors, Cushing syndrome, obesity, and other conditions.
- The National Centers for Translational Research in Reproduction and Infertility (formerly the Specialized Cooperative Centers Program in Reproduction and Infertility Research) is a national network of NICHD Fertility and Infertility Branch (FIB)–supported research-based centers that aims to promote interactions between basic and clinical scientists with the goal of improving reproductive health. Several centers focus on diseases/disorders of the female reproduction system that may affect women who have undergone treatment for tumors in Cushing syndrome.
 BACK TO TOP
BACK TO TOP