Basic information for topics, such as "What is it?" and "How many people are affected?" is available in the About Labor and Delivery section. Answers to other Frequently Asked Questions (FAQs) specific to labor and delivery are in this section.
 "False labor" refers to irregular contractions that sometimes happen before true labor begins. These contractions are also called Braxton Hicks contractions. It can be hard to tell the difference between Braxton Hicks contractions and true labor contractions.
"False labor" refers to irregular contractions that sometimes happen before true labor begins. These contractions are also called Braxton Hicks contractions. It can be hard to tell the difference between Braxton Hicks contractions and true labor contractions.
The following chart, from the American Congress of Obstetricians and Gynecologists, shows some ways that Braxton Hicks contractions differ from true labor contractions.1
| Type of Change | False Labor | True Labor |
|---|---|---|
| Timing of contractions | Contractions do not come regularly and do not get closer together. | Contractions come at regular times and get closer together over time. Each lasts about 30 to 70 seconds. |
| Effect of movement | Contractions may stop when the woman walks or rests, or they may stop when the woman changes position. | Contractions continue despite movement. |
| Strength of contractions | Contractions are usually weak and do not get much stronger or they may start strong and get weaker. | Contractions get steadily stronger. |
| Pain of contractions | The woman usually feels pain only in the front. | Pain usually starts in the back and moves to the front. |
When women carry multiple fetuses―twins, triplets, or quadruplets, for example―labor and delivery proceed through the same stages as with a single infant. But labor and delivery with multiples has some important differences. For example, women having multiples are more likely to have certain complications.2 The most common are preterm labor and preterm birth.
Preterm labor is labor that starts before 37 weeks of pregnancy. It can result in preterm birth. More than half of all twins are born preterm. Preterm infants can have problems with breathing and eating and may have to stay in the hospital longer than other infants.
In a pregnancy with multiples, providers look to see whether the woman has one or more than one placenta, which direction(s) the fetuses are facing, and where the umbilical cords lie. In addition, they closely monitor the woman's health, because carrying multiples can increase a woman's risk of gestational diabetes and preeclampsia. These factors can all affect when and how a provider recommends delivering the babies. Some of these complications may require a cesarean delivery to resolve. Multiples are about 2.5 times more likely to be delivered by C-section than singletons are.2,3
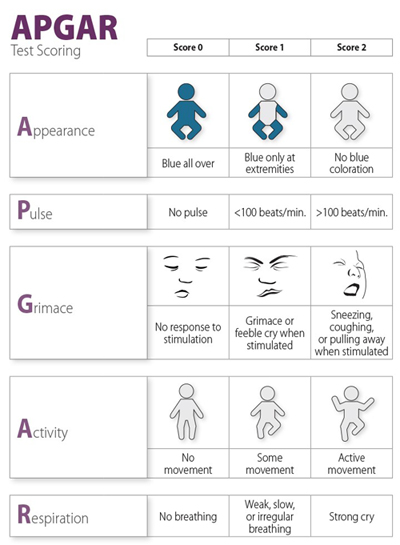
The Apgar test, performed 1 minute and 5 minutes after birth, gauges an infant's overall health. A health care provider assesses the following aspects of an infant's health:
- Skin color
- Heart rate
- Reflexes (response to stimulation, such as a mild pinch)
- Muscle tone
- Breathing
Based on this examination, the health care provider gives the infant an Apgar score of 1 to 10. The higher the score, the better the infant is doing.4
Women older than 35 are at higher risk for preterm labor and preterm birth. Preterm infants can have serious short- and long-term health problems.
Older women are also more likely to have a stillbirth, which is when a fetus dies in the uterus after 20 weeks of pregnancy.
Women in their 30s are also more likely than younger women to need a cesarean delivery.5
Although most women give birth in hospitals, some families choose a home birth or birth in an out-of-hospital birthing center.6 The American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (ACOG) recommend births in hospitals or birthing centers as the safest options.7
Talk to your health care provider about where you want to deliver your baby. If possible, schedule a time to visit the hospital, birthing center, or other setting before you make your decision. Consider the risks and benefits of each as you make your decision.
Women who are good candidates for home birth:7
- Are generally in good health
- Have not had a previous cesarean delivery
- Do not have pregnancy-related health problems or illness
- Do not have multiples
- Have a fetus with good size and health
- Have a fetus in the head-down position
- Go into labor at 37 weeks or later
Planned home births benefit from having the following resources in place:7
- A certified nurse-midwife, certified midwife, or practicing physician
- At least one appropriately trained individual whose primary responsibility is the care of the newborn infant
- Quick access to health care providers who can provide consultation if complications happen
- A reliable plan for safe and fast transportation to a nearby hospital in case of an emergency
The American Association of Birth Centers maintains a list of accredited locations. Find a birth center near you .
Some women report that being immersed in water during early labor shortened their labor and reduced their pain. However, these and other benefits of giving birth in water are unconfirmed by research evidence. Also, water births carry risks, including infections and drowning. The American College of Obstetricians and Gynecologists notes that allowing women to labor in a birthing pool may have benefits, but it recommends against giving birth in water. Visit OB/GYNs Weigh In: Laboring in Water is OK, but Deliver Baby on Land for more information.8
Labor and birth are considered preterm, or "premature," if they occur before 37 weeks of pregnancy. Preterm labor and birth share many features with regular labor and delivery, but they also have unique features. For this reason, preterm labor and preterm birth are addressed in a separate topic.
Citations
- American College of Obstetricians and Gynecologists. (2011). FAQ: How to tell when labor begins. Retrieved February 3, 2017, from http://www.acog.org/Patients/FAQs/How-to-Tell-When-Labor-Begins
- American College of Obstetricians and Gynecologists. (2015). FAQ: Multiple pregnancy. Retrieved February 3, 2017, from http://www.acog.org/Patients/FAQs/Multiple-Pregnancy
- Osterman, M. J. K., & Martin, J. A. (2013). Changes in cesarean delivery rates by gestational age: United States, 1996–2011. NCHS Data Brief, 124, 1–8.https://www.cdc.gov/nchs/products/databriefs/db124.htm
- MedlinePlus. (2014). Apgar score. Retrieved February 3, 2017, from http://www.nlm.nih.gov/medlineplus/ency/article/003402.htm
- American College of Obstetricians and Gynecologists. (2015). FAQ: Having a baby after age 35: How aging affects fertility and pregnancy. Retrieved February 3, 2017, from https://www.acog.org/womens-health/faqs/having-a-baby-after-age-35-how-aging-affects-fertility-and-pregnancy
- MacDorman, M. F., Mathews, T. J., & Declercq, E. (2014). Trends in out-of-hospital births in the United States, 1990–2012. NCHS Data Briefs, 144, 1–8.
- American Academy of Pediatrics. (2013). Policy statement: Planned home birth. Retrieved February 3, 2017, from http://pediatrics.aappublications.org/content/early/2013/04/24/peds.2013-0575
- American Academy of Pediatrics, & American College of Obstetricians and Gynecologists. (2016). Committee opinion: Immersion in water during labor and delivery. Retrieved February 7, 2017, from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2016/11/immersion-in-water-during-labor-and-delivery

 BACK TO TOP
BACK TO TOP