The illustrations below show how the human placenta develops. The timeline of placental development shows how the placenta changes over the course of pregnancy. A crucial stage of placental development is when blood vessels in the lining of the uterus are remodeled, increasing the supply of blood to the placenta. This process, called spiral artery remodeling, is also illustrated in close-up.
Placental Development: Fertilization to Full Term
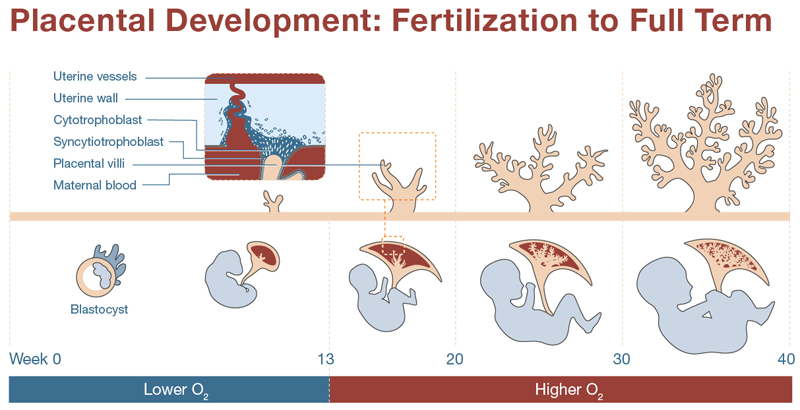
This timeline compares development of the fetus and the placenta across 40 weeks of pregnancy. Between Weeks 0 and 13, the fertilized blastocyst embeds in the uterine wall, and development of the fetus and placenta begin. At this time, the placenta is a relatively low-oxygen environment. Placental villi are lined with cells known as cytotrophoblasts and syncytiotrophoblasts. The cytotrophoblasts breach the uterine wall and begin reshaping blood vessels there. These remodeled vessels become a source of maternal blood for the placenta. The placenta develops to bring oxygen and nutrients to the fetus and to move harmful waste and nutrients away. Over time, the villi develop increasingly dense branching to accommodate the increased demand of the developing fetus.
Spiral Artery Remodeling
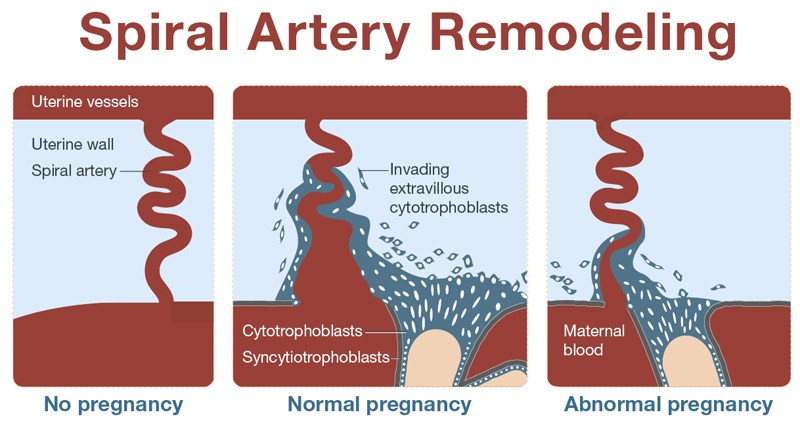
Spiral arteries in the uterine wall are remodeled to supply blood to the fetus during pregnancy. When there is no pregnancy, the spiral artery spans the tissue of the uterine wall, supplying blood to the lining. In a normal pregnancy, cytotrophoblast cells from placental villi invade the space around the spiral artery, replacing cells which normally line the vessel. This remodeling makes the vessel larger and optimizes the blood flow to the placenta to support its function. In an abnormal pregnancy, cytotrophoblasts invade the space in and around the spiral artery, but the artery is not completely remodeled and blood flow from the mother to the placenta is not optimized to support proper placental function.
 BACK TO TOP
BACK TO TOP