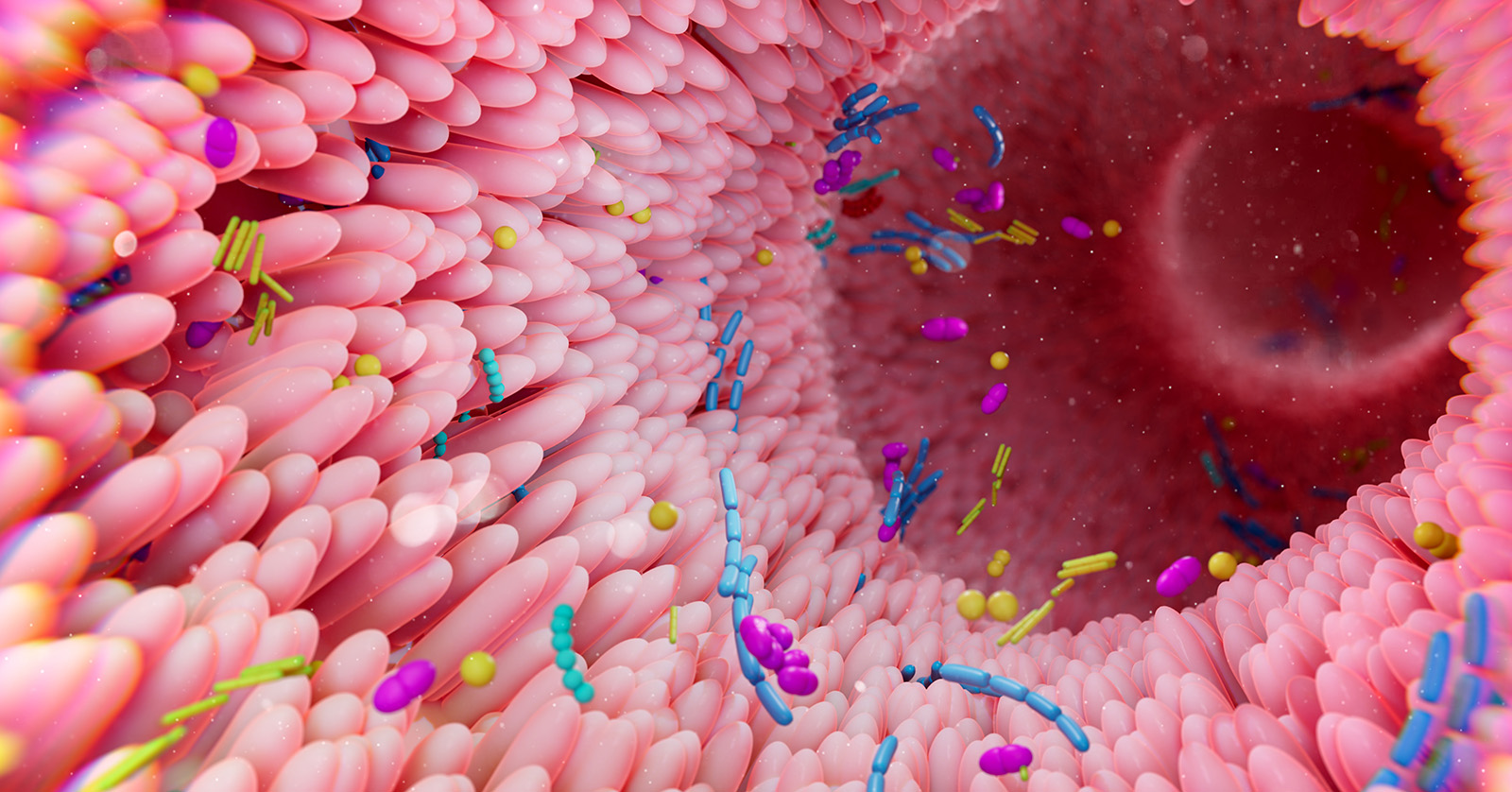
Failure of the microbiome to fully establish itself in an infant’s digestive system precedes the development of a subtype of necrotizing enterocolitis (NEC), a life-threatening illness that disproportionately affects preterm infants, according to a study funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The microbiome is the community of microorganisms that live in a particular part of the body, such as the gastrointestinal tract. The researchers found that this type of NEC is preceded by a low-diversity microbial community and occurs 40 or more days after birth among infants born in the 23rd to 25th week of pregnancy.
The researchers also found that changes to preterm infant gut microbiomes are associated with drug treatments, including antibiotics, and the microbiomes often were colonized by microorganisms found in hospitals. The results may inform efforts to understand and prevent NEC and other conditions affecting preterm infants.
The study was conducted by Phillip I. Tarr, M.D., Gautam Dantas, Ph.D., and Barbara B. Warner, M.D., of Washington University School of Medicine, and their colleagues. It appears in Cell Host and Microbe.
Background
Newborns acquire the microbes that populate their gut microbiomes from their mothers and their environment. Factors that influence microbiome development include the manner of delivery (vaginal or cesarean birth), exposure to antibiotics, diet (breast milk or formula), and gestational age at birth. Preterm infants often undergo intensive hospital care, which may include treatment with antibiotics and many additional medications. Variations in how preterm infants’ microbiomes develop are thought to influence their risk for NEC and infections of the bloodstream.
Results
For the current study, researchers identified the gut microbiome by analyzing genomes present in stool samples. The team evaluated samples, collected from multiple timepoints, from 236 preterm infants hospitalized during the first three months of life in three U.S. newborn intensive care units.
The microbiomes of term infants develop gradually and are populated by organisms that aid digestion, contribute nutrients, and tend not to cause harm. In contrast, preterm infant microbiomes from the study tended to initiate with Staphylococcus epidermis, a bacterium normally found on the skin, but which can cause infections when it occurs in other tissues.
The researchers confirmed earlier findings that up to 50 percent of preterm infants’ microbiome communities consist of pathobionts—microbes normally present in the host but can cause diseases under certain conditions. Over several weeks, the preterm infant microbiome communities transitioned from S. epidermis to other pathobionts, including Klebsiella pneumoniae, Enterococcus faecalis, and Escherichia coli.
The researchers identified a subtype of NEC that developed after 40 days among infants born from 23 to 25 weeks of pregnancy who had a gut microbiome containing a low diversity of organisms. However, the authors found no difference between the patterns of microorganisms in the digestive system of infants who did not develop NEC and those who developed NEC earlier than the 40th day of life.
The investigators also found that preterm infants shared certain strains of gut bacteria, which suggests that these organisms were acquired in the newborn intensive care unit. In addition to strains of S. epidermis, infants in the same intensive care unit also shared strains of Clostridioides difficile, a bacterium which can cause severe diarrhea and intestinal inflammation in adults. Moreover, specific strains of S. epidermis were found in infants treated in intensive care units from three U.S. states, which the authors believe suggests that the strains were adapted to survive in the hospital environment and in infant digestive systems.
Treatment with antibiotics was associated with large-scale changes in preterm infant microbiomes. However, the study could not determine if the antibiotic treatment caused the changes or were given in response to a change. Similarly, treatment with non-antibiotic drugs, such as antacids, also were associated with changes in preterm microbiomes.
Significance
The authors concluded that their findings provide a framework for future studies on how gut microbial communities might contribute to medical disorders affecting preterm infants.
Reference
Thanert, R, et al. Clinical sequelae of gut microbiome development and disruption in hospitalized preterm infants. Cell Host and Microbe. 2024.

 BACK TO TOP
BACK TO TOP