The first step in diagnosing MD is a visit with a healthcare provider for a physical exam. He or she will ask a series of questions about the person’s family history, including any family members with MD, and medical history, such as muscle problems the person may be experiencing.
Different tests can help healthcare providers diagnose MD and determine which type of MD is present. The tests also may rule out other problems that could cause muscle weakness, such as injury, toxic exposure, medications, or other muscle diseases. These tests may include:1
- Blood tests to measure levels of certain substances that may be high in someone with MD. Elevated levels of these substances can signal muscle weakness, injury, and disease and point to a need for additional testing. Some of these may include:
- Serum creatine kinase, an enzyme released into the bloodstream when muscle fibers are damaged
- Serum aldolase, an enzyme that helps break down sugars into energy
- Myoglobin, a protein that carries and stores oxygen in muscles
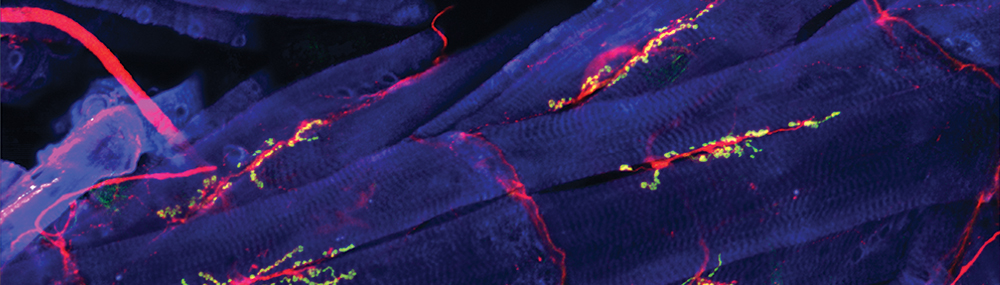
- Muscle biopsies, which involve the removal of a small piece of muscle tissue using a needle or small incision. Providers examine the tissue under a microscope to check for hallmarks of MD. Patients diagnosed by muscle biopsy usually need genetic testing as well to confirm mutations in their genes.2
- Genetic testing to look for genes known either to cause or be associated with inherited muscle disease. DNA analysis and enzyme assays can confirm the diagnosis of certain neuromuscular diseases, including MD.
- Neurological tests to rule out other nervous system disorders, identify patterns of muscle weakness and wasting, test reflexes and coordination, and detect contractions.
- Heart testing, such as an electrocardiogram (ECG), to measure the rate and frequency of heartbeats, or echocardiogram (Echo), to measure the force of heartbeats and look at the structure of the heart. Some forms of MD cause heart problems such as an irregular heartbeat.3
- Exercise assessments to measure the patient’s muscle strength and breathing and detect any increased rates of certain markers following exercise.
- Imaging tests such as magnetic resonance imaging (MRI) and ultrasound imaging, which use radio waves/magnetic fields and sound waves, respectively, to take pictures of the inside of the body, examine muscle quality and bulk, and measure fatty replacement of muscle tissue.
For more information about diagnosing MD, visit the National Institute of Neurological Disorders and Stroke website Muscular Dystrophy: Hope Through Research.
 BACK TO TOP
BACK TO TOP